Marking the World Rabies Day
With The Drug Information Centre (DIC) of
The Pharmaceutical Society of Nigeria (PSN)
The 28th of September every year has been set aside by the World Health Organisation (WHO) to draw attention to rabies. The Drug Information Centre (DIC) of the Pharmaceutical Society of Nigeria (PSN) joins the ‘celebration’ by raising awareness with current information on the disease and highlighting progress made in defeating it.
INTRODUCTION
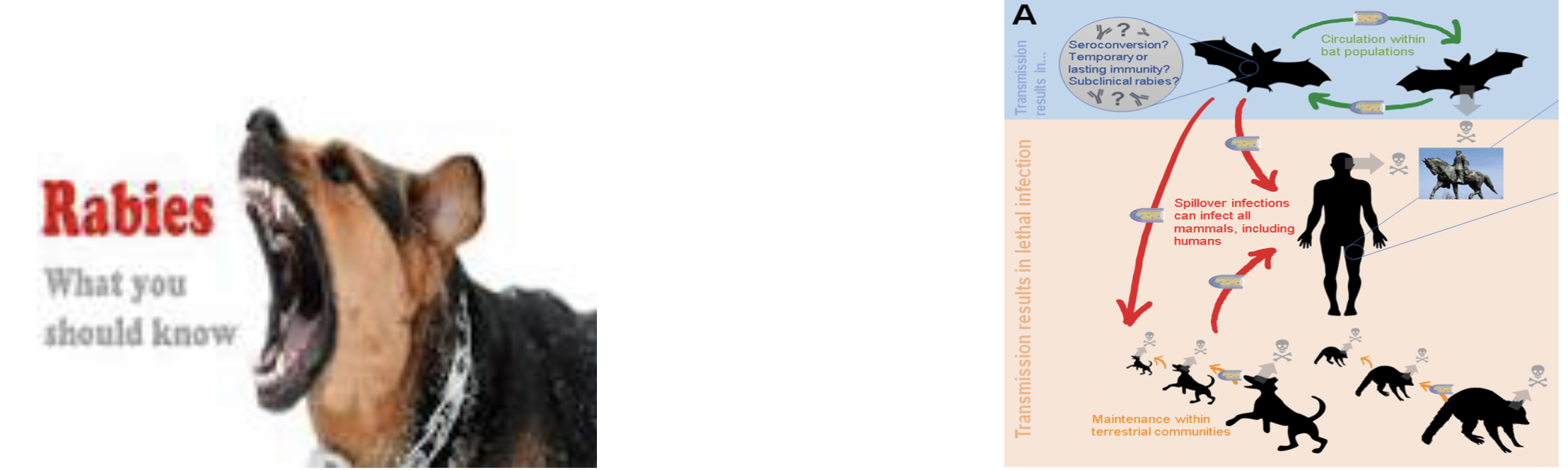
Rabies, also known as Hydrophobia and Lyssa, is one of the neglected vaccine-preventable viral diseases. It has been recognised for over 4,000 years and occurs in nearly all countries, affecting poor and vulnerable populations who live in remote and rural locations. The risk of rabies is highest in countries with hyperendemic canine rabies, including most of Asia, Africa and Latin America. 95% of human deaths from rabies occur in Asia and Africa (Russel and Brown, 2021). Rabies is most often transmitted through the bite of rabid, wild and domestic animals. The rabies virus causes the disease in the brain of mammals – encephalomyelitis – and may lead to death by infecting the central nervous system (CNS).
The vast majority of rabies cases reported to the American Centres for Disease Control and Prevention each year occur in wild animals like bats, raccoons, skunks and foxes, although any mammal can get rabies (CDC, 2022). Fatality is 100%, the vast majority occurring in developing countries.
Nigeria, known for rabies endemicity, records approximately 55,000 deaths from it each year, from human rabies infected by rabid dogs, Dogs account for about 94% of confirmed human infections. In up to 99% of cases in Nigeria, domestic dogs are responsible for rabies virus transmission to humans (WHO, 2021)..
RABIES VIRUS
Rabies virus is of the Rhabdoviridae family, which includes at least three genera of animal viruses: Lyssavirus, Ephemerovirus, and Vesiculovirus. They belong to the order Mononegavirales, viruses with a nonsegmental, negative-stranded RNA genomes. The genus Lyssavirus includes Lagos bat, Mokola virus, Duvenhage virus, European bat virus 1 & 2 and Australian bat virus.
It is a rod- or bullet-shaped, single-stranded, negative-sense, unsegmented, enveloped RNA virus. The virus genome encodes five proteins. All species of mammals are susceptible to rabies infection.
INFECTION PROCESS
Rabies is spread via the virus-laden saliva of an infected animal through a bite or saliva contact with mucous membranes or a fresh break in the skin. It is NOT transmitted through contact with blood, urine, skunk spray, or faeces of an infected animal.
There are five general stages of rabies infection in humans: incubation, prodrome, acute neurologic period, coma and death.
The incubation period is extremely variable, ranging from less than 10 days to longer than 2 years, the commonest being 1–3 months. This period is shorter in children and in people exposed to a large dose of the rabies virus.
What happens is that the viral RNA uncoats in the cytoplasm of infected cells. The genome is transcribed by a virion-associated RNA-dependent RNA polymerase. Viral RNA is then translated into individual viral proteins. Replication occurs with synthesis of positive-stranded RNA templates for the production of progeny negative-stranded RNA.
Rabies virus then travels through the nerves to the spinal cord and brain.
 The prodrome period is the period between when the symptoms start and ends when the patient either recovers or dies from the disease. It usually lasts 2-10 days, characterised by flu-like, nonspecific complaints such as fatigue, headache, fever, pain and numbness/tingling at the site of the bite.
The prodrome period is the period between when the symptoms start and ends when the patient either recovers or dies from the disease. It usually lasts 2-10 days, characterised by flu-like, nonspecific complaints such as fatigue, headache, fever, pain and numbness/tingling at the site of the bite.
The virus is highly sensitive to both the active and passive immune responses of the host before entering into the nerve endings adjacent to the site of viral multiplication. However, if not destroyed at the site of infection, the neurotropic virus migrates centrally via peripheral unmyelinated nerves at a rate estimated between 10 and 400 mm/day (Jackson AC, 1999). It then spreads centrifugally to numerous other organs.
During the acute neurologic period, the virus binds to the nicotinic acetylcholine receptors at the neuromuscular junction, travelling through the retrograde axonal transport, acting like a neurotoxin. This results in the patient usually suffering paralysis; disorientation and hallucinations; episodes of terror and excitement; hyperventilation; hydrophobia; hypersalivation; and seizures. These symptoms are invariably followed by severe inflammation of the brain and spinal cord, cerebral dysfunction, after which the person deteriorates rapidly into coma and death. Once symptoms have begun, there is usually no treatment or cure. Prevention is the only tool.
DIAGNOSIS
Questions to ask victims:
- What animal bit you?
- Was it a wild animal or a pet?
- If it was a pet, do you know who owns the pet?
- Was it vaccinated?
- Can you describe the animal's behaviour before it bit you?
- Was the animal provoked?
- Were you able to capture or kill the animal after it bit you?
What to do immediately after being bitten
- Wash your wound gently and thoroughly with soap and generous amounts of water. This may help wash away the virus.
- If possible, capture or contaoin the animal that bit without further causing more injury. Do not kill the animal with a blow or a shot to the head, as the resulting injuries may make it difficult to perform laboratory tests to determine whether the animal has rabies.
- Contact the local health department to determine what to do with the animal.
Early diagnosis of human rabies is difficult. It is usually suggested by epidemiologic and clinical findings and confirmed in the laboratory. The diagnosis is however less difficult if there is a history of animal bite exposure and if a full spectrum of symptoms and signs has appeared. Rabies should be suspected in human cases of unexplained viral encephalitis with a history of animal bite. The failure to suspect rabies in several of the recent human deaths in the United States may have occurred because no thorough exposure history had been sought. Unvaccinated persons are often negative for virus-neutralizing antibodies (VNA) until late in the course of disease.
Laboratory Diagnosis
Rabies may be established if rabies antigen, antibody, viral RNA, or the isolation of virus are detected. Serial serum specimens for detection of rabies antibodies, saliva specimens for culture of virus and skin biopsies for direct immunofluorescence testing for virus antigen are sometimes necessary, especially when rabies is strongly suspected. This is because any single, individual test may give false negativeresult.
Performing a direct immunofluorescence test on a skin biopsy from the nape of the neck is one of the most rapid methods to diagnose rabies antemortem in humans as evidence of rabies antigen. Direct immunofluorescence test is the most sensitive and specific method of detecting rabies antigen in skin and other fresh tissue (e.g., brain biopsy), although the results may occasionally be negative in early stages of the disease (Rupprecht CE, 1996).
Positive Indicators for Rabies:
- Nonspecific prodrome prior to onset of neurologic signs
- Neurologic signs consistent with encephalitis or myelitis
- Dysphagia
- Hydrophobia
- Paresis
- Progression of neurologic signs
- Negative test results for other aetiologies of encephalitis(CDC 2008).
Negative Indicators for Rabies:
- Improvement or no change in neurologic status
- Illness with at least 2-3 weeks duration
TREATMENT
Rabies shots include:
- A rapid-acting injection (of rabies immune globulin) protecting people from rabies is given to people that have not received rabies vaccine as soon as possible after the bite, near the area where the animal bit the victim.
- A series of prophylactic rabies injetions that help the body to learn to identify and fight the rabies virus is given to those that have not previously had the rabies vaccines. They receive four injections over 14 days of human diploid cell vaccine (HDCV) or purified chick embryo cell vaccine (PCECV) 1.0 mL, IM (deltoid area ), one each on days 0 , 3, 7 and 14. Those that have previously had the rabies vaccine get two injections over the first three days.
[A 5th dose on day 28 may be recommended for immunocompromised persons]
Rabies Vaccines
- RabAvert rabies vaccine (produced by Bavarian Nordic)
- IMOVAX rabies vaccine (produced by Sanofi Pasteur)
Human Rabies Immune Globulins
- KEDRAB (produced by Kedrion Biopharma)
- HyperRab (produced by Grifols)
- Imogam (produced by Sanofi Pasteur)
(CDC, 2020)
CONTROL
Though the best prevention of rabies is by avoiding exposure to it, what will control this zoonotic disease is vaccination of susceptible animal species, particularly dogs and cats.
When an exposure is suspected, efforts should be made to determine whether an exposure actually occurred and whether a risk of rabies exists in the geographic area. If treatment (postexposure prophylaxis) is necessary, it should be initiated promptly. Postexposure prophylaxis consists of the combination of local wound cleansing, HRIG and rabies vaccine.
Reference
- Can J Infect Dis. 2002 Mar-Apr; 13(2): 121–125. doi: 10.1155/2002/475909WHO Regional Office for Africa 2021. https://www.afro.who.int/news/nigeria-joins-world-raising-awareness-rabies
- CDC. Human Rabies Prevention—United States, 2008, Recommendations of the Advisory Committee on Immunization Practices (ACIP), MMWR. May 23, 2008; 57:RR-03
- CDC. Vaccine and Immune Globulin Availability. https://www.cdc.gov/rabies/resources/availability.html Page last reviewed: August 24, 2020
- Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of High-Consequence Pathogens and Pathology (DHCPP) http://www.cdc.gov/ Page last reviewed: November 30, 2020
- Jackson AC. Case 21-1998: rabies. N Engl J Med 1999;340:65
- Olivier Despond, MD, Marisa Tucci, MD FRCPC, Hélène Decaluwe, MD, Marie-Claude Grégoire, MD, Jeanne S Teitelbaum, MD FRCPC, and Nathalie Turgeon, MD FRCPC
- Rupprecht CE. Rhabdoviruses: Rabies Virus. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 61. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8618/
- Russell Katherine and Brown Kevin 2021. GOV-9720 (previously GW 1536) www.ukhsa.gov.uk © Crown copyright 2021 version 7